April 2016
Case Presentation
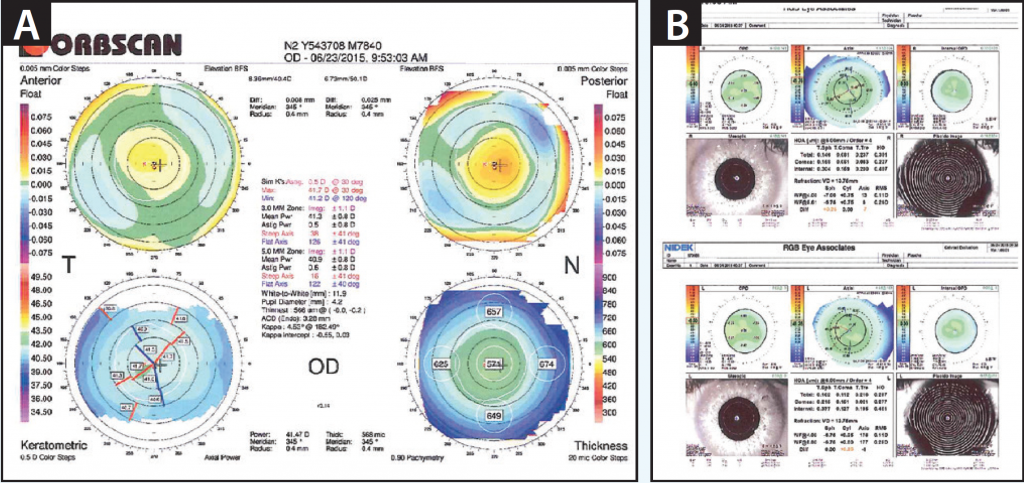
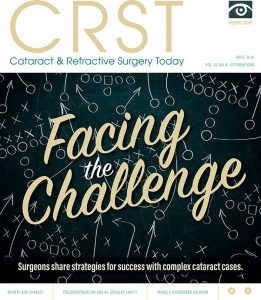
Figure 1. Preoperative measurements with the Orbscan (A) and the OPD-Scan III (B).
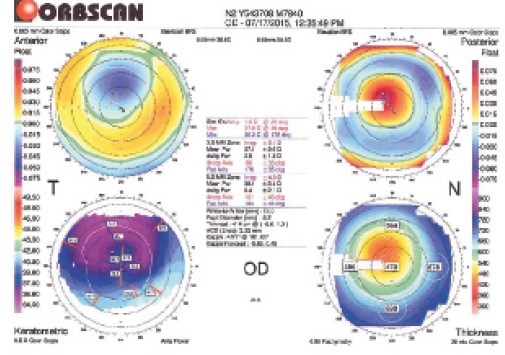
Figure 2. Orbscan measurements taken 9 days after LASIK.
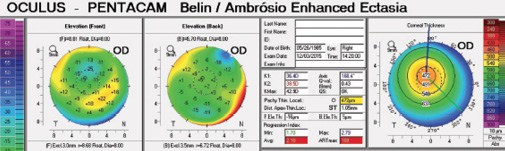
Figure 3. Measurements taken with the Pentacam Comprehensive Eye Scanner approximately 5 months postoperatively.
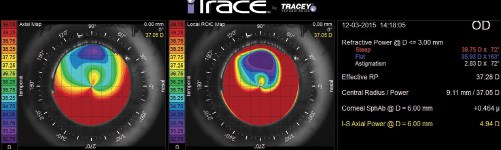
Figure 4. Measurements taken with the iTrace (Tracey Technologies) approximately 5 months postoperatively.
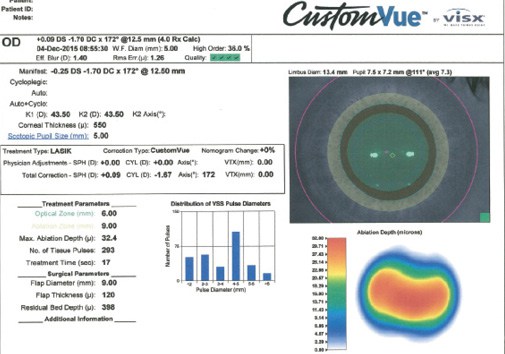
Figure 5. Advanced CustomVue treatment plan guided by the WaveScan WaveFront System (both from Abbott Medical Optics). Note the total ablation of 32.4 μm.
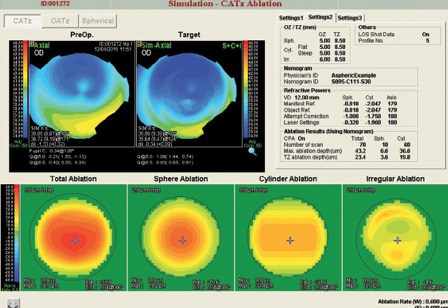
Figure 6. CATz (Custom Aspheric Treatment Zone; Nidek) plan processed by Final Fit, based on OPD-Scan III topography. Note the ablation for irregularity in the bottom right corner planning for 12.3 μm of irregular ablation (with a total of 56.7 μm of ablation).

JAMES S. LEWIS, MD
This patient with high myopia had normal corneal pachymetry readings, regular topography (average keratometry readings of 41.00 D OU), and no relevant ocular, family, or social history. Despite both eyes’ perfect appearance at the slit lamp postoperatively, he described the vision in his right eye as blurry. One week postoperatively, the manifest refraction was -2.75 +2.25 X 90 OD with a BCVA of 20/25- versus near plano and 20/20 OS. Orbscan topography (Bausch + Lomb) suggests a 3-mm superiorly decentered ablation. The corneal morphology rules out inadvertent ablation of the flap’s posterior surface, which can occur in such cases.
My recommendation is to use the irregularity ablation pattern shown in Figure 6. Nidek’s Final Fit Software can address these challenging cases with topography-guided treatment. The simulated axial map shows a predicted enlargement of the central optical zone. My preference would be to lift the flap and treat only the 12.3-µm irregularity component at this stage (off label). I caution patients that a second and sometimes a third retreatment may be needed. Fortunately, this patient has plenty of residual stroma, a normal flap, and a healthy left eye.
I have treated more than a dozen patients with this degree of irregularity and many more with higher degrees of topographic abnormality. The results have been encouraging.

CHARLES R. MOORE, MD
The preoperative measurements with the Orbscan and OPD-Scan III (Nidek) appear to be normal and show myopic astigmatism. The problem is a result of a decentered ablation superiorly and possible ablation inside the superior edge of the flap. This produced irregular cylinder, coma, and poor-quality vision. My suggestion would be to refer this patient for topography-guided PRK (or a LASIK relift) to someone with a lot of expertise in treating this type of complication. An alternative would be to consider Intacs (Addition Technology), but in my experience with this sort of problem, topography-guided results are superior. This case is a classic example of why patient fixation is necessary even with an eye tracker.

ASIM PIRACHA, MD
Figure 1A shows regular astigmatism and sufficient central corneal thickness for the treatment of his refractive error. He lost 1 line of BCVA after LASIK.
The postoperative measurements, visual acuity, and refraction are consistent with a decentered ablation that, although rare, can still occur with modern excimer laser systems. The patient has a residual compound myopic astigmatic refractive error and increased irregular corneal astigmatism. The surgical procedure was noted to be routine without flap-related complications, a decentered or small-diameter flap, or poor fixation.
To further evaluate this patient, I would perform an overrefraction with a rigid gas permeable lens and testing with the iTrace to confirm that the loss of BCVA is due to the irregular astigmatism or decentered ablation. If the patient’s BCVA improved with the overrefraction and the iTrace showed low internal aberrations, then either a wavefront-guided or a topography-guided ablation could be considered. I would confirm that the manifest refraction and topography were stable before proceeding with further treatment.
In this case, my preference would be topography-guided surface ablation to conserve tissue, treat corneal aberrations on the cornea, expand the optical zone, and center the treatment over the corneal apex rather than the pupil. Because it can only flatten the cornea and does not combine hyperopic and myopic ablations to correct the higher-order aberrations, wavefront-guided treatment would further flatten an already flat cornea and remove a greater amount of tissue from a thinned cornea.
The only topography-guided treatments available in the United States use the Allegretto Wave Eye-Q (Alcon) and Nidek EC-5000 CXII (Nidek) lasers. These treatments are approved for LASIK on normal corneas, however, not for irregular postsurgical astigmatism. Thus, topography-guided ablation would be an off-label use of the laser in this case. The patient should be fully informed and understand prior to treatment that the primary purpose of surgery is to improve his BCVA and not necessarily his UCVA. He should also understand that a second surface ablation procedure might be needed to correct any residual refractive error.

WHAT I DID: WILLIAM F. WILEY, MD
The patient was referred to me for confirmation of the diagnosis of a decentered ablation and treatment recommendations. Based on the postoperative topography, I confirmed the diagnosis. Analysis for wavefront- and topography-guided ablation approaches was performed to help me determine the most appropriate treatment recommendation (Figures 5 and 6). The Final Fit software (Nidek) displays the irregular portion of the proposed ablation pattern prior to surgery. This allowed me to compare the proposed irregular treatment with the corneal topography to determine if the ablation pattern matched the corneal irregularity. Furthermore, with topography-guided ablation, I can see the anticipated postoperative topographic appearance prior to surgery to ascertain if it will be an improvement over the pre-enhancement topography.
In this case, the anticipated topography showed potential improvement (Figure 6), and the irregularity treatment pattern correlated with the elevation maps shown on the Pentacam Comprehensive Eye Scanner (Oculus Surgical; Figure 3). Topography-guided LASIK has been reported to yield an improvement in irregular astigmatism,1 which I discussed with the patient along with the potential need for multiple surgeries to achieve a satisfactory outcome.
The patient chose to proceed with an enhancement. I lifted the flap and performed topography-guided ablation. On postoperative day 1, the patient had a UCVA of 20/20, and his symptoms had improved. I await further follow-up and postoperative topography results. n
1. Gatinel D, Bains HS. Treatment of highly aberrated eyes using the Nidek CXIII excimer laser. J Refract Surg. 2010;26(6):453-457.
Section Editor Alan N. Carlson, MD
• professor of ophthalmology and chief, corneal and refractive surgery, Duke University Eye Center, Durham, North Carolina
Section Editor Stephen Coleman, MD
• director of Coleman Vision, Albuquerque, New Mexico
Section Editor Karl G. Stonecipher, MD
• clinical associate professor of ophthalmology, University of North Carolina, Chapel Hill
• director of refractive surgery, TLC in Greensboro, North Carolina
Section Editor William F. Wiley, MD
• private practice at Cleveland Eye Clinic, Cleveland, Ohio
• (440) 526-1974
• financial disclosure: consultant to Abbott Medical Optics and Alcon
James S. Lewis, MD
• private practice, Elkins Park, Pennsylvania
• (215) 886-9090; jslewis@jameslewismd.com
• financial interest: none acknowledged
Charles R. Moore, MD
• medical director, International EyeCare Laser Center, Houston
• (713) 984-9777; crm@texaslasik.com
• financial interest: none acknowledged
Asim Piracha, MD
• medical director, Cornea, Cataract and Refractive Surgery Service, John-Kenyon Eye Center, Louisville, Kentucky
• associate professor, Department of Ophthalmology and Visual Sciences, University of Louisville, Louisville, Kentucky
• (502) 895-2910; apiracha@johnkenyon.com
• financial disclosure: member of the speakers’ bureau for Abbott Medical Optics

